December 6, 2024
This article first appeared in Sedgwick's Recall Index 2024 Edition 2.
Reduce impacts and enable quick response by understanding your quality and risk management processes
In today's world where medical devices have become increasingly complex, it is critical that device manufacturers fully understand their quality and risk management processes to minimize the chance of a product recall.
Medical device recalls are frequently reported in the news. While this may raise concerns about the impact on safety for products relevant to daily life, it is important to know the key elements of the recall framework to understand the impact individuals or a community may experience.
Recall processes will need to keep evolving as CDRH continues to strengthen postmarket surveillance activities and the medical device recall program and medical devices continue to increase in complexity.
As part of postmarket surveillance, medical device manufacturers monitor internal production data and external complaint data. They can use health hazard evaluations and other tools to identify safety signals to identify a side effect or adverse event that is potentially caused by the device. From there they can determine if a recall is needed.
For example, a manufacturer may consider the degree to which a product's possible deficiency is obvious to the user. Based on those considerations, the device maker will determine whether the device did not function as intended or if it was not used as intended — was it a product error or a user error? Finally, the manufacturer will assess whether potential risks posed by the device could result in theoretical harm or real harm to patients.
The role of GAO
In the past, the U.S. Congress has requested that the Government Accountability Office (GAO) investigate activities related to recall practices. In 1998, GAO explored whether the Food and Drug Administration ensures that manufacturers operate systems that are capable of tracking devices through the distribution chain to end users. The office also looked into whether device manufacturers and FDA are executing recalls of tracked devices in a timely manner.
In 2011, Congress asked GAO to follow up on its 1998 findings. In the 2011 report, GAO determined that FDA "has not routinely analyzed recall data to determine whether there are systemic problems underlying trends in device recalls." It also found that the agency is "missing an opportunity to use recall data to proactively identify and address the risks presented by unsafe devices."
Now, in 2024, some members of Congress have once again asked GAO to explore FDA's recall processes. Partially due to GAO's earlier findings, FDA has implemented modifications to continuously improve recall processes for the medical device industry. A new GAO report might show if the agency has done enough.
Interestingly, the only mention of safety signals in FDA's Center for Radiological Health (CDRH) Strategic Priorities for 2022-2025 is a success metric stating that by Dec. 31, 2025, FDA identify and act on safety signals related to medical devices first or in coordination with regulatory agencies of other major markets more than 75% of the time.
Recalls over the last 10 years
A retrospective review of medical device recalls shows the extent and type of recalls over the last ten years. FDA's recall dashboard shows a total of 10,535 medical device recalls in fiscal years (FY) 2014-2023, Oct. 1, 2013, through Sept. 23, 2023. Of those, 541 (5.1%) events were classified as Class I; 9,554 (90.7%) were Class II; and 440 (4.2%) were Class III recalls.
These results echo the findings reported by GAO in 2011, in which nearly 83% of all the recalls from calendar years 2005-2009 were Class II recalls. The 499 medical device recalls categorized as Class II in 2023 was more than 2020-2022 combined, which had a total of 489. The COVID-19 pandemic may have been a significant factor in the lower numbers.
Reasons for Class I recalls in this timeframe included issues related to software, battery functionality, contamination, IFU (Warnings), materials, electrical issues, thermal issues, sterility, manufacturing, and lack of FDA authorization for marketing. Examples of devices that did not have market authorization included COVID-19 tests or related diagnostics during the 2021-2022 period.

Regulatory developments
CDRH recently published its 2024 CDRH Safety Report. The publication contains, among other things, efforts for strengthening postmarket surveillance and the medical device recall program.
For postmarket surveillance, FDA highlights the existing Unique Device Identifier (UDI) System, including the creation of the Global Unique Device Identification Database (GUDID) containing a list of all UDIs. Eighty percent of medical device reports include a product's UDI, allowing for better tracking of devices throughout the total product lifecycle.
FDA states that part of CDRH's vision is that "U.S. postmarket surveillance quickly identifies poorly performing devices, accurately characterizes real-world performance, and facilitates device approval or clearance." The realization of these vision statements may be a focus of future GAO investigations.
To illustrate its efforts to strengthen the medical device recall program, FDA mentions the numerous guidance documents it has issued to help medical device manufacturers ensure the devices are safe and effective. The agency also highlighted its work to increase recall data transparency, including the public FDA recall dashboard.
Part of FDA's 2024 actions are focused in the postmarket setting, with tasks to "strengthen active surveillance" including focus on real-world evidence (RWE). As defined by FDA, RWE refers to clinical evidence about the usage and potential benefits or risks of an FDA regulated product derived from analysis of real-world data.
Additionally, efforts to enhance the medical device recall program, with goals to reduce the time between when FDA becomes aware of a recall and the public is notified about the event, are included in the safety report.
As medical devices evolve in complexity and add software and connectivity features, software- and cybersecurity-prompted recalls are becoming more prevalent.
Challenges ahead
The challenges to global supply chain networks impact many industries. Medical device manufacturers often find themselves identifying and qualifying additional sources of materials and components to avoid potential disruptions. However, multiple sources of materials and components potentially complicate the tracing of subcomponents and materials that could be related to root causes that impact device performance and safety.
Having robust traceability records and systems that readily link devices to specific component and/or material vendors will provide medical device manufacturers with the speed and precision needed to identify potentially affected devices. It also fulfills the manufacturer's obligations under the Quality System Regulation, which requires traceability mechanisms be in place.
As medical devices evolve in complexity and add software and connectivity features, software- and cybersecurity-prompted recalls are becoming more prevalent. This prevalence is expected to continue to increase. Identifying software and connectivity issues early to ensure safety and functionality of medical devices will become more challenging as devices become more sophisticated.
One challenge of recalls continues to be the notification process for accounts or end users and their associated effectiveness checks. Efforts to move recall notifications to a digitized platform were the focus of a recent public meeting held by FDA.
Faster recall notifications and a system that provides a digital interface may speed the process and add efficiencies to get medical devices pulled from inventory and prevent the use of a faulty device. There are digital platforms currently in development to reduce the time of public notification once FDA becomes aware of a recall.
Future considerations
Recall processes will need to keep evolving as CDRH continues to strengthen postmarket surveillance activities and the medical device recall program and medical devices continue to increase in complexity.
FDA recently highlighted the success of medical device manufacturers participating in the Voluntary Improvement Program (VIP). This initiative includes an appraisal of quality system maturity in reducing the overall number of Class I recalls since 2018. As this program evolves, it will be interesting to monitor if quality system maturity appraisals are instituted in the future for all medical device makers.
Another factor to consider is that many medical devices are distributed globally, thus compounding the logistical challenges of recalls. A robust internal recall plan and the ability to engage in mock recalls to confirm systems and team members are ready to execute can strengthen a manufacturer's readiness. This can also provide the opportunity to enhance or modify processes over time to accelerate preparedness for when an actual recall occurs.
Being able to respond quickly and accurately will be important to how both regulators and patients view the company.
What Can We Help You Solve?
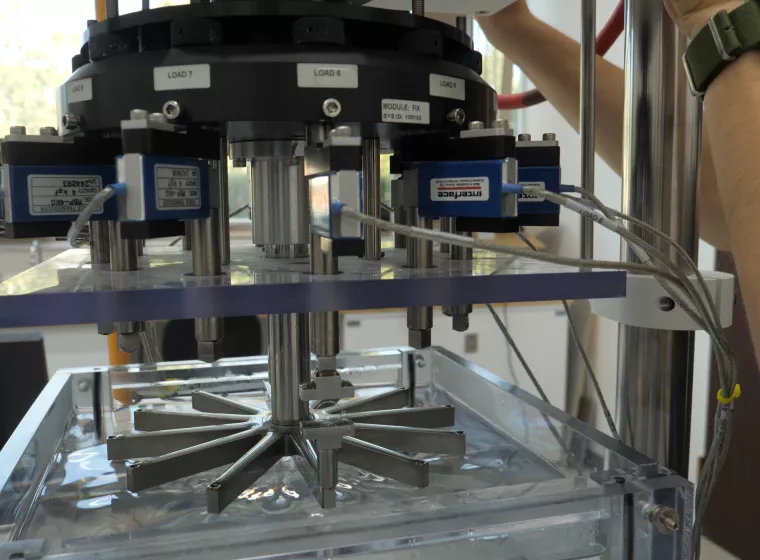
Exponent's biomedical engineers and regulatory experts are experienced in every facet of medical device design, including design verification, usability studies, electrical medical equipment configuration, software review, and laboratory testing. We support clients in addressing product claims and recalls, helping you select and implement appropriate corrective and preventive actions.





![Medical Devices, Implants & Surgical Tools [MCE]](/sites/default/files/styles/cards_home_card/public/media/images/GettyImages-1182458826.jpg.webp?itok=z7lVBn-v)

![[MCE] [BES] Medical Device Development Support - a tray of surgical tools](/sites/default/files/styles/cards_home_card/public/media/images/GettyImages-1296782647.jpg.webp?itok=N2clVZFq)
![Medical Devices [EECS]](/sites/default/files/styles/cards_home_card/public/media/images/GettyImages-523306516.jpg.webp?itok=4e0Y2HMn)